Crisis Intercept Maps for Service Members, Veterans, and their Families
What’s
at Stake
Veterans die of suicide at a disproportionate rate. In 2018, 13.8 percent of all U.S. adults who died of suicide were Veterans, even though they make up just 8 percent of the country’s adults (U.S. Department of Veterans Affairs, 2020, U.S. Census Bureau, 2020). Most of these were not getting help from the federal agency that serves Veterans. Only 35 percent of Veterans who died of suicide were in contact with the Veterans Health Administration (Veterans Health Administration, 2017). That means that services provided in the community are an important way to reach and help Veterans who are at risk. Suicide is a public health crisis. Community support is essential in reducing the number of Veterans who take their lives.
Our Solution
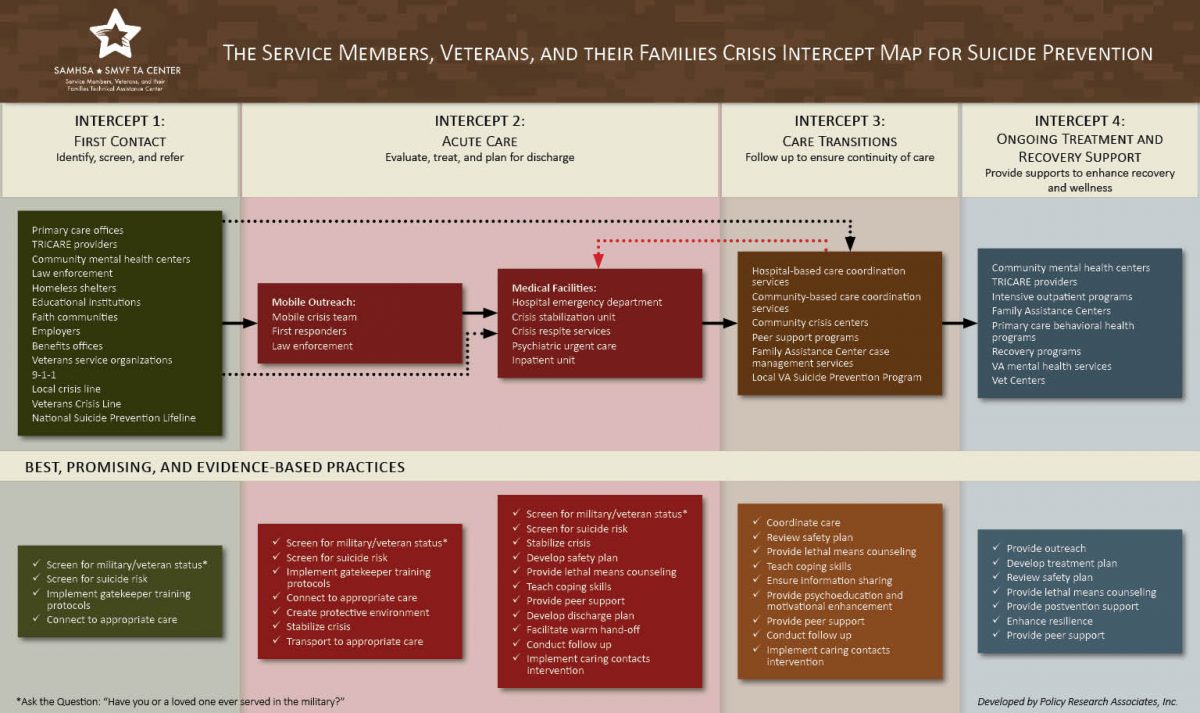
The Crisis Intercept Map for Service Members, Veterans, and their Families or SMVF is a targeted mapping service. It helps behavioral health and Veterans’ services work together better. Through this mapping, attendees explore how to enhance suicide prevention, crisis care, and post-vention services for SMVF. Through the Crisis Intercept Mapping process, decision-makers develop an action plan to strengthen the crisis care continuum for SMVF. The Crisis Intercept Map focuses on the following:
- Strengthening community-based behavioral health systems
- Breaking down siloes between agencies
- Increasing access to culturally competent, comprehensive, and continuous care
Each Crisis Intercept Map for SMVF is customized to the unique needs of the community. However, our team of facilitators will guide each site through these general steps:
- Become oriented to the mapping process through introductory phone calls
- Develop an attendance list of critical decision-makers for the meeting
- Collect data on available services
- Develop a profile of the community, so that attendees can apply the crisis map to their work
- Attend a 1- to 1.5-day Crisis Intercept Map meeting
- Work collaboratively to build a map of the local crisis system for SMVF
- Use the map to develop an action plan for changes to address gaps and overlaps in services
Our Model
Policy Research Associates, Inc. developed the Crisis Intercept Map. Its purpose is to help communities support SMVF who experience thoughts of suicide, also known as suicidal ideation. The Crisis Intercept Map prioritizes the following targets for SMVF in mental health crisis:
- Meeting SMVF where they are in the community
- Delivering acute care
- Offering follow-up assistance when an individual is still at high risk
The Crisis Intercept Map outlines the flow of SMVF experiencing thoughts of suicide through behavioral health services. The mapping focusses on four specific intercepts, or moments when help could be provided:
- First contact. The people in need are identified, screened, and directed to the appropriate service providers (e.g., crisis hotlines, emergency departments).
- Acute care. Service providers assess, treat, and plan to release SMVF from care (e.g., local hospitals).
- Care transitions. Providers offer follow-ups and ensure continuity of care (e.g., Veterans service organizations).
- Ongoing treatment and recovery support. Stakeholders provide support to enhance the recovery and wellness of SMVF (e.g., trauma recovery programs).
Stakeholders
The stakeholders involved in the Crisis Intercept Map for SMVF include:
- Medical centers
- Veterans service organizations and trauma recovery programs
- Local mental health and substance use treatment services
- Local law enforcement agencies
- Crisis hotlines, local hospitals, and emergency departments
- Local, state, and federal departments of Veterans affairs
Examples / Case Studies
Examples/Case Studies
Our trained team of facilitators are experts in delivering this cross-systems mapping. We have served 27 communities across the country in the last 3 years.
Virginia, 2018
The Commonwealth of Virginia hosted a Crisis Intercept Map for SMVF in 2018. Attendees included representatives from the Virginia Department of Veterans Services, the Department of Behavioral Health and Developmental Services, the Department of Social Services, hospitals, healthcare associations, Virginia’s U.S. Department of Veterans Affairs medical centers, and the Virginia National Guard. Working together, the team established three goals (known as the “3 Cs”):
- Care: Provide culturally competent and accessible behavioral health and support services
- Connect: Bring services together to form partnerships
- Communicate: Educate community members and service providers on military culture and available resources
To implement the 3 Cs, Virginia launched a pilot that ran from February to September 2020. The pilot embedded military culture, suicide prevention, and safety planning resources in state and community agencies.
Virginia also made SMVF resources more accessible during key windows. They focused this work on pre-crisis services and life-saving services during a crisis. Between February and April 2020, the pilot program served 2,048 people and screened 64 percent of them for suicide risk. They found that 23 percent of the 1,305 individuals they screened were “at risk.”
In the future, the program plans to expand suicide risk screening and referrals and improve data quality. It will also promote the expansion and future operation of these activities by finding multiple sources of funding.
Houston, Texas, 2017
Roughly 300,000 Veterans live in or near Houston, Texas. Mayor Sylvester Turner wanted to expand the conversation around SMVF mental health and suicide. Mayor Turner also wanted to strengthen partnerships between local communities, governments, and nonprofit agencies. The city held a Crisis Intercept Map for SMVF in July 2018. The assembled team looked at care coordination across the crisis continuum. Using the resulting map, the team partnered with the Harris Center and the Michael E. DeBakey VA Medical Center. Together, they established a robust and continuous care coordination model for Houston-based SMVF.
Follow-Up Assistance
Follow-up technical help is not always needed after your cross-systems mapping event. But some jurisdictions find additional assistance useful. If your community wants more support, the Systems Mapping Center is here. The Center can host follow-up meetings, give guidance and resources, or connect you with topic experts. These follow-up opportunities are offered on a fee-for-service basis if the need comes up.